|
Thinking skills are such an important part of your child’s development. Good thinking skills can help your child make good choices, come up with creative ideas and try to solve their problems independently.
Here are 10 simple techniques you can use throughout the day to stimulate your child’s thinking skills: 1. Schedule ‘free-time’: This may seem counter-intuitive. Children growing up in Bangkok usually go from school to a series of after-school lessons. While this stimulates a child’s learning and gives them new skills, it is important to realize that this is all structured time with little opportunities to think independently. So, try to leave a daily time open in your child’s schedule for unstructured ‘free time’. 2. Pretend-play: Play serves as an important foundation for thinking and language. When your child pretends during play, they learn to associate a toy, or a pretend-event, with a real object or a real event. Pretend-play helps your child think about the world around them and understand it better. 3. Limit and rotate toys: Good news – there is no need to constantly buy new toys. No matter how many toys you buy, your child will eventually become bored of all of them. Instead, keep toys the same and rotate the toys, every few days. Encourage your child to use these same toys to create new situations or to use them in new ways. For example, your child can use a toy-rock as a phone during play, or use a sheet of paper as a blanket. This is called substitution-play and it is great for expanding your child’s thinking through their imagination. 4. Familiar stories with new endings: More good news – you also do not have to keep buying new books. Yes, your child might become familiar with the stories that you read to them, or that they have started reading by themselves. But, you can keep these books interesting by stopping half-way or towards the end and asking your child, “how do you want the story to end this time? Why do you want this to happen?” This will make your child think more than if they are simply listening to a story. 5. Stop and Wait: When your child has a question or a small problem, it is intuitive to immediately step-in and help. Instead, try to stop and wait first. This will give your child the chance to think for themselves and attempt to solve their problem creatively or independently. By assuming competence, you empower your child to think independently. 6. Teach reasons, as well as rules: During speech therapy sessions, I usually explain the reason behind each rule I give. I have found that this helps children understand the purpose of rules, which makes them more likely to follow the rules. So, the next time you give your child a rule, try to explain the reason why this rule exists. You might be surprised at how they respond once you expand their thinking and understanding this way. 7. Ask open-ended questions: Questions like ‘why’, ‘how’ and ‘what if’ will help your child to expand their thinking and creativity. One way you can do this is after watching a movie together. For example, “why do you think this happened in the movie?” Another way you can do this is when your child asks you for something, “why do you want a new bike?” 8. Think out loud: You can model thinking to your child by thinking out loud. You can do this throughout the day during your routines or when you make a decision. For example, before leaving home together, “look at the clouds in the sky, it’s going to rain today. I think we should take the umbrella”. 9. Teach a second language: Research studies have shown that being bilingual has many cognitive benefits, including improved memory, ability to learn new things and flexibility between tasks. Interestingly, there is research showing that the cognitive benefits of being bilingual start from the young age of 7-months (Kovacs & Mehler, 2009) . 10. Finally, encourage your child to ‘explore’ their surroundings outside. After all, thinking and creativity is limited between four walls! Speak soon, The Expat Speechie Reference: Kovacs, A., & Mehler, J. (2009). Cognitive Gains in 7-month old Bilingual Infants. PNAS, 106, 6556–6560. Last month, I travelled back to Australia for the next level of PROMPT Training. Honestly speaking, when I did the PROMPT Introductory Course in Australia a couple of years ago, I never imagined how much impact PROMPT Therapy would have on the communication development of some of the children I work with. These children and teenagers did not have any words before they started PROMPT Therapy – and now they are saying their first words, even at the age of 16! And the best part about it is that the children, even the really young kiddos, understand the value of PROMPT Therapy. Anyone who is a Parent or Educator knows that when the child is on board, any learning is possible.
Here are 3 powerful insights from PROMPT: 1. Most children benefit from engaging more than one sensory system in learning. Children are often expected to learn to speak through exposure in their environment, or by being explicitly taught things verbally - both of these methods rely mostly on a child's ability to learn new information auditorily. However, for many children, this is not the best way for them to learn. Research evidence has shown that some children learn to communicate better when information is visually presented, such as with pictures, hand-signs, and written words. Now, this is where PROMPT shines. PROMPT is a unique approach to teaching communication because not only does it involve engaging a child auditorily and visually, but it also relies heavily on using tactile cues (applying touch and pressure to a child's face). By teaching children to communicate by using these three different cues at the same time, we give children more tools to succeed. 2. Turn-taking is important in all communication exchanges. Even though PROMPT focuses heavily on speech-sound production and speech clarity, turn-taking is a must in every activity. By working on speech production in turn-taking activities, children also practice this core non-verbal communication skill in all of their communication exchanges. Also, when the activity involves turns, a child has the chance to listen to the correct verbal model provided when it is not their turn. Most children enjoy learning during turn-taking activities because it alleviates them from the 'pressure to perform', since the focus of the activity is not always on them. In my experience, teaching communication is also more fun with turn-taking! 3. Communication is made up of sub-systems; by improving one sub-system you can change other sub-systems. PROMPT is more about the bigger picture when it comes to improving a child's communication. Rather than just focusing on one area of communication, such as speech sounds, PROMPT Therapy always involves working on at least two of the communication sub-systems below at the same time:
I am looking forward to continue seeing more first words, and other words to follow through the use of PROMPT Therapy. If you would like to know more about PROMPT, you can read more about it in my introduction post about PROMPT by clicking here. Speak soon, The Expat Speechie Chiman Estephan, MSLP, MSPA, CPSP, ACAS In 2010, the ESDM was named “top 10 medical interventions” by TIME Magazine.
This month's post was written by guest writer, Dr. Plern Pratoomas. Dr. Plern is an Early Intervention and Child Development Specialist, who is currently the only ESDM Certified Trainer in Thailand. When Dr. Plern first introduced the ESDM for children with Autism to me, I was left in awe. Many children who I work with have Autism, and the more I learned about the ESDM, the more I realised how beneficial this could be for their overall development. If you would like to know more about the ESDM, you can read about it below. Speak soon, The Expat Speechie What is the Early Start Denver Model (ESDM)? The ESDM is an intervention designed to address the challenges faced by young children with Autism. The overarching goal of ESDM is to bring the child back into the social world so they can engage in social learning. ESDM therapy prioritizes the building blocks required for social learning - by teaching early interaction skills such as imitation, joint attention, communication, and turn-taking, ESDM therapy aims to fill in the developmental gaps that are commonly seen in children with Autism. The ESDM uniquely combines two different approaches by blending together developmental principles and behavioral teaching techniques into one comprehensive intervention program. The ESDM is developmental in its approach, as it is grounded in developmental research and how typical children learn and grow. However, the ESDM is also behavioral because it incorporates teaching techniques and procedures from the field of Applied Behavior Analysis (ABA). At its core, the ESDM is relationship-based, which means that the way in which ABA teaching procedures are used in therapy is very natural and a heavy focus is on back-and-forth engagement, social communication, and social interaction. The ESDM uses a trans-disciplinary approach because Autism impacts all areas of a child’s development. One team member acts as a “team lead” and is responsible for providing the intervention, while experts from other fields provide ongoing feedback and consultation. In essence, there is only one treatment plan that incorporates a multidisciplinary perspective. This approach streamlines intervention for the family and ensures that the therapist focuses on the integration of skills across different developmental domains. What does the ESDM offer that other programs do not? The ESDM is manualised with clear instructions and guidelines on assessment, teaching content, and teaching procedures. The ESDM is curriculum-based, which means that results from the assessment (“ESDM Curriculum Checklist”) determine the goals and objectives that an ESDM therapist will choose to target in the intervention. To ensure standardization of treatment and therapist skills, the ESDM has an ESDM Teaching Fidelity Rating System to measure and maintain the quality of therapy implementation. All of the above ensures that ESDM intervention is both customized to each child’s needs but standardized in regard to quality and content. If you are more familiar with social-developmental interventions (e.g. DIR/Floortime, SCERTS, RTI), the ESDM might seem too behavioral. If you are more familiar with behavioral interventions, the ESDM may seem too developmental. Since ESDM is a unique blend of these two approaches, it is important to note the ways in which the ESDM is different from other interventions. The ESDM differs from most developmental interventions in these ways:
When comparing the ESDM to other behavioral approaches (e.g. Discrete Trial Training or other traditional ABA programs), ESDM is different in these ways:
What does ESDM therapy look and feel like? If you were to walk into an ESDM therapy session at its best, you would see:
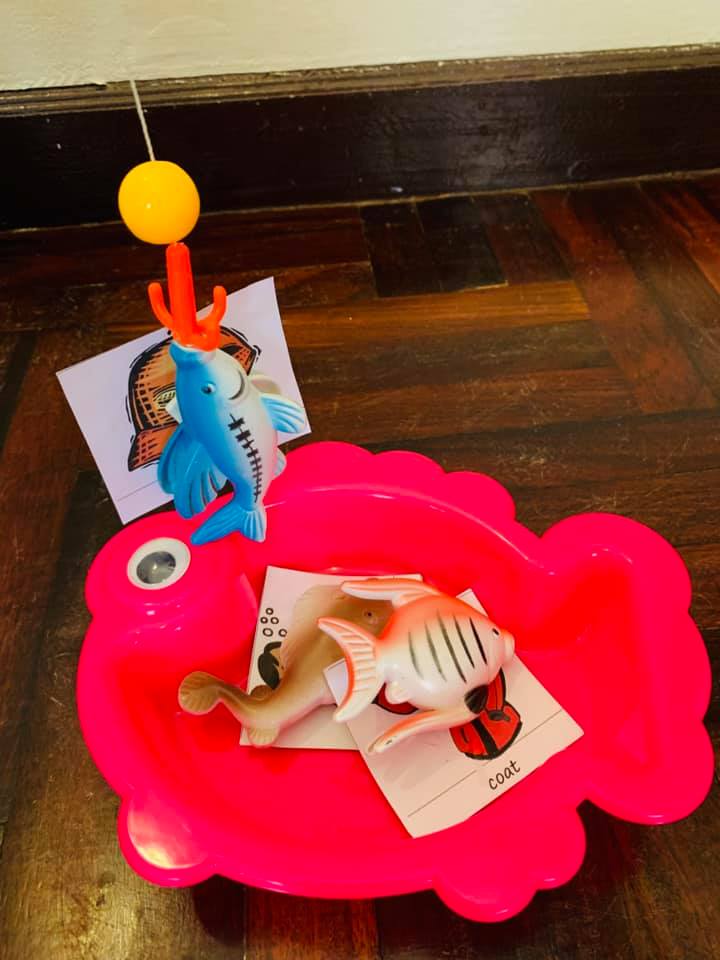
Where does ESDM therapy take place? ESDM therapy can take place across many locations, including in the family’s home, at school/daycare, or out in the community. Who is the ESDM for? As an early intervention program, the ESDM was developed to be used with infants, toddlers, and preschoolers with Autism. Children as young as 1 year old up to the age of 5 years can benefit from ESDM therapy. Who delivers ESDM treatment? The treatment can be delivered by a range of early childhood professionals (e.g. Special Education, ABA, Speech and Language Therapy, Physical Therapy, Occupational Therapy, Psychology) or trainees who work with children with Autism and who have read the ESDM manual can deliver ESDM treatment within their own practice. However, ESDM Certified Therapists have been through additional, more rigorous training and have met fidelity of implementation with multiple children. What is the effectiveness of the ESDM for young children with Autism? There is a growing body of research that demonstrates the effectiveness of ESDM intervention. For a list of published articles, please visit: https://www.esdm.co/research-articles Finally, if you are a parent and think that the ESDM might be a good fit for your child, please contact Little Sprouts Children's Centre to inquire about Thailand’s first official ESDM program (managed and supervised by an interdisciplinary team of professionals, including supervision and training by an ESDM Certified Trainer). If you are a professional and would like to pursue formal training and/or ESDM certification, please contact Plern Pratoommas at [email protected]. For more information about the official ESDM training/certification process, please visit: www.esdm.co This article was written by Dr. Plern Pratoomas, Early Intervention and Child Developmental Specialist, ESDM Certified Trainer and Therapist. Reference: Rogers, S. J., & Dawson, G. (2010). Early Start Denver Model for Young Children with Autism: Promoting Language, Learning, and Engagement. Guilford Press.  Have you ever tried having a conversation with someone whose eyes were fixated on the TV? Your conversation probably didn’t get very far. What if that person wanted you to see / join in what they were watching on TV, so they constantly shifted their eye gaze between you and the TV? They probably would have been able to take in more of what you were saying then. This is known as 'joint attention'. It’s the same with children. Joint attention is when a child divides their attention between an object and another person. For example, if your child looks at their toy bear, looks up at you, as if to say “look!” and then looks back at their toy bear. When does joint attention develop? Children typically start to develop joint attention at the age of 9 months, and continue to do so until mastering the skill at the age of about 18 months. Why is joint attention so important? This shared attention and engagement serves as a foundation for learning - otherwise, learning doesn’t happen. Joint attention must be mastered for children to develop good communication, cognitive and social skills. On the other hand, children who have difficulty with joint attention will usually struggle with many areas of development. Here are some important things to remember: In children's development, non-verbal communication skills develop before verbal communication skills. Since joint attention is a non-verbal communication skill, it must be worked on before working on verbal communication skills in therapy. Below are 5 of my favorite tricks for improving your child’s joint attention: 1. Start with what your child is interested in For example, your child will be more keen to interact with you when you show interest in the toy car that they are interested in - rather than the alphabet puzzle which you keep asking them to do. 2. Guide your child’s eyes For example, if your child is interested in a toy, bring this toy slowly up to your eyes, and then slowly put it back down. This will help guide your child about where to look. Since you are starting with the toy that they are interested in, their eye gaze will likely follow your hand movements. 3. Go with the pace your child is setting For example, if your child is making car sounds while they play with a car toy, you can make car sounds too! Try not to break the momentum by placing demands on your child (e.g. "say car! say it!"). 4. Use environmental sounds to draw your child in For example, your child might enjoy it when you make some animal sounds as you both play with the animal toys together. 5. Remember the aim of your interaction The aim is to achieve shared attention and engagement - not to force your child to say everything you want them to say. The greater the demands you put on them, the less motivation they will have to engage with you. I hope you find these tips helpful when working on your child's joint attention. Speak soon, The Expat Speechie Chiman Estephan MSLP, MSPA, CPSP, ACAS © Copyright 2019. The Expat Speechie www.theexpatspeechie.com. All Rights Reserved.  Children love to play games. You can play many games with your child which create fun opportunities for supporting their speech development. When working on a child's speech, one of the tools I use are 'picture cards'. This is because most children learn better with visual support. Picture cards are simply cards with pictures of objects with the target speech sounds which a child is working on. For example, below are picture cards which I've used to teach children to say the 'c' sound at the beginning of words. There are plenty of picture cards (for all sounds of the English language) which you can download free on the internet, or you can even make your own picture cards with your child as a fun and creative activity at home. Once you have your child's picture cards ready, here are my 8 favourite speech games below, which you can play with your child: 1. Word hunt: You can do this at home by hiding the cards around the room. When your child finds a card, they can practice saying the word in a short sentence with the correct sounds. 2. Games with counters: Start by turning the picture cards face down on the table. Take turns to flip a card over and place a counter (use a different colour for each person's counters) on the card when the sounds are produced correctly in the word. Once every card has a counter on it, count who has the most counters on the cards - that person wins. 3. Ball games: Thinking of words that start with a target sound before taking a turn to throw / kick the ball. 4. Bowling: stick one picture card on each bowling pin. Each time your child takes a turn at bowling, they can practice saying the words on the pins that fall down.  5. Post-it: Your child can make a 'post-box' at home, where they can 'post' a picture card each time they say the word correctly. 6. Magic bag: You can start by placing all the cards in a bag. Then taking turns to pull one card out while closing your eyes. Practice saying the word on the picture cards in a sentence. 7. Fishing: Place a piece of Velcro on the back of each picture card and on the bottom of each fishing rod. Take turns ‘fishing’ for a picture card. Each time you catch a picture, practice saying the word in a phrase.
8. Memory matching: For this you will need two copies of the picture cards. Turn the cards over so that the pictures can’t be seen. Then take turns turning over two cards each, saying the words on each card and keeping the pairs that match. Playing games with picture cards are a great way to stimulate and support your child's speech development at home. Taking turns during these games will give your child constant modeling, as well as opportunities to practice saying their sounds correctly in words and sentences. Have fun and speak soon! The Expat Speechie Happy New Year Parents!
|
Welcome to my blog!
|